KRAS G12C IS CHALLENGING
PATIENTS WITH KRAS G12C MAY FACE RAPID PROGRESSION AND NEED ALTERNATIVE TREATMENT OPTIONS1-3
For over 40 years, KRAS had been challenging to target due to the protein’s smooth surface providing few binding pockets for small molecules, and high binding affinity for GTP.4,5
See 3 reasons why KRAS G12C may require a treatment that can challenge its relentlessness in advanced NSCLC.
GTP=guanosine triphosphate; NSCLC=non-small cell lung cancer.

KRAS G12 IS A PREVALENT DRIVER MUTATION WITH POOR PROGNOSIS1-3,6-10

The presence of a KRAS G12C mutation in advanced NSCLC is correlated with poorer prognosis in patients treated with chemotherapy when compared to patients with KRAS wild type.3,7
Some studies have shown that second-line+ treatment with docetaxel in patients with KRAS G12C–mutated NSCLC is associated with a median real-world PFS of less than 5 months8-10
ALK=anaplastic lymphoma kinase; BRAF=B-Raf proto-oncogene; EGFR=epidermal growth factor receptor; HER2=human epidermal growth factor receptor 2; MET=mesenchymal epithelial transition; NTRK1=neurotrophic tyrosine receptor kinase; PFS=progression free survival; PIK3CA=phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha; RET=rearranged during transfection; ROS1=proto-oncogene C-Ros1, receptor tyrosine kinase.

Prevalence of specific driver mutations in lung adenocarcinoma1,6

METASTASES IN NSCLC ARE COMMON11-14
- 40% of patients with KRAS G12C-mutated NSCLC developed brain metastases11*
~50% of patients with NSCLC and brain metastases were asymptomatic12†
~30%-40% of patients with lung cancer develop bone metastases during the course of their disease13,14

*Based on retrospective analysis of patients with KRAS G12C-mutated advanced nonsquamous NSCLC (n=65) from a large tertiary referral center.11
†In a single-center prospective observational study of treatment-naïve patients with NSCLC (N=496); brain metastases were detected in 104 (21%); 53 (51%) were asymptomatic.12

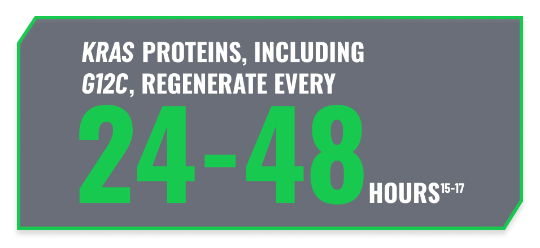
CONTINUOUS REGENERATION MAY REQUIRE CONTINUOUS INHIBITION15-17
- KRAS G12C mutations produce abnormal KRAS proteins that lead to aberrant signaling and uncontrolled cellular proliferation18-20
- KRAS G12C may need to be continuously inhibited to suppress tumorigenesis15-17

References:
- Pakkala S, Ramalingam SS. Personalized therapy for lung cancer: striking a moving target. JCI Insight. 2018;3(15):e120858.
- Acker F, Stratmann J, Aspacher L, et al. KRAS mutations in squamous cell carcinomas of the lung. Front Oncol. 2021;11:788084.
- Hames ML, Chen H, Iams W, et al. Correlation between KRAS mutation status and response to chemotherapy in patients with advanced non-small cell lung cancer. Lung Cancer. 2016;92:29-34.
- Ghimessy A, Radeczky P, Laszlo V, et al. Current therapy of KRAS-mutant lung cancer. Cancer Metastasis Rev. 2020;39(4):1159-1177.
- Lu S, Jang H, Muratcioglu S, et al. Ras conformational ensembles, allostery, and signaling. Chem Rev. 2016;116(11):6607-6665.
- Nassar AH, Adib E, Kwiatkowski DJ. Distribution of KRASG12C somatic mutations across race, sex, and cancer type. N Engl J Med. 2021;384(2):185-187.
- Svaton M, Fiala O, Pesek M, et al. The prognostic role of KRAS mutation in patients with advanced NSCLC treated with second- or third-line chemotherapy. Anticancer Res. 2016;36(3):1077-1082.
- Iams WT, Balbach ML, Phillips S, et al. A multicenter retrospective chart review of clinical outcomes among patients with KRAS G12C mutant non-small cell lung cancer. Clin Lung Cancer. 2023;24(3):228-234.
- Gray JE, Hsu H, Younan D, et al. Real-world outcomes in patients with KRAS G12C-mutated advanced non-small cell lung cancer treated with docetaxel in second-line or beyond. Lung Cancer. 2023;181:107260.
- de Langen AJ, Johnson ML, Mazieres J, et al. Sotorasib versus docetaxel for previously treated non-small-cell lung cancer with KRASG12C mutation: a randomized, open-label, phase 3 trial. Lancet. 2023;401(10378):733-746.
- Cui W, Franchini F, Alexander M, et al. Real world outcomes in KRAS G12C mutation positive non-small cell lung cancer. Lung Cancer. 2020;146:310-317.
- Naresh G, Malik PS, Khurana S, et al. Assessment of brain metastasis at diagnosis in non–small cell lung cancer: a prospective observational study from north India. JCO Glob Oncol. 2021;7:593-601.
- Al Husaini H, Wheatly-Price P, Clemons M, Shepherd FA. Prevention and management of bone metastases in lung cancer: a review. J Thorac Oncol. 2009;4(2):251-259.
- D’Antonio C, Passaro A, Gori B, et al. Bone and brain metastases in lung cancer: recent advances in therapeutic strategies. Ther Adv Med Oncol. 2014;6(3):101-114.
- Stites EC, Shaw AS. Quantitative systems pharmacology analysis of KRAS G12C covalent inhibitors. CPT Pharmacometrics Syst Pharmacol. 2018;7(5):342-351.
- Shukla S, Allam US, Ahsan A, et al. KRAS protein stability is regulated through SMURF2: UBCH5 complex-mediated β-TrCP1 degradation. Neoplasia. 2014;16(2):115-128.
- Bergo MO, Gavino BJ, Hong C, et al. Inactivation of Icmt inhibits transformation by oncogenic K-Ras and B-Raf. J Clin Invest. 2004;113(4):539-550.
- Fernández-Medarde A, Santos E. Ras in cancer and developmental diseases. Genes Cancer. 2011;2(3):344-358.
- Cox AD, Fesik SW, Kimmelman AC, Luo J, Der CJ. Drugging the undruggable RAS: mission possible? Nat Rev Drug Discov. 2014;13(11):828-851.
- Waters AM, Der CJ. KRAS: the critical driver and therapeutic target for pancreatic cancer. Cold Spring Harb Perspect Med. 2018;8(9):a031435.


